Kentucky Pesticide Safety Education Program

Questions?
Contact
Dr. Ric Bessin
Dept. of Entomology
University of Kentucky
859-257-7450
rbessin@email.uky.edu
Toxicity, Exposure, and Hazard
Pesticides are chemicals designed to be toxic to certain groups of organisms so that they can control pest species effectively. Use them very carefully to avoid harming yourself, others, and non-target organisms.
 Pesticides can have acute (short-term) and chronic (long-term) health effects. The signal word on the product label and the information contained in the Hazards to Humans and Domestic Animals part of the Precautionary Statements section of the label indicate the toxicity concerns and list the minimum personal protective equipment (PPE) and precautions needed to reduce risk when using the product. Pesticides also can pose additional physical and chemical hazards by being explosive and/or combustible. Information on physical or chemical hazards of products is included in the Precautionary Statements section. In addition, the Safety Data Sheet (SDS) has much more information on toxicity and precautions.
Pesticides can have acute (short-term) and chronic (long-term) health effects. The signal word on the product label and the information contained in the Hazards to Humans and Domestic Animals part of the Precautionary Statements section of the label indicate the toxicity concerns and list the minimum personal protective equipment (PPE) and precautions needed to reduce risk when using the product. Pesticides also can pose additional physical and chemical hazards by being explosive and/or combustible. Information on physical or chemical hazards of products is included in the Precautionary Statements section. In addition, the Safety Data Sheet (SDS) has much more information on toxicity and precautions.
Toxicity is a measure of the ability of a pesticide to cause acute or chronic injury or illness.
It is a combination of its chemical properties and concentration or amount.
Exposure occurs when pesticides get on or into the body through the skin, lungs, mouth, or eyes. There is great risk of exposure when: opening and handling containers; mixing and loading concentrates; working around or repairing contaminated application equipment; making applications; cleaning up spills; and re-entering a recently treated area before the spray has dried.
Hazard or risk is the potential or probability for harm (injury, illness, or allergy) to occur from the combination of the product's toxicity and the level of exposure to it. Product formulations differ greatly in their exposure risk. As an applicator, you can reduce your risk by choosing a less-toxic product or formulation, by reducing exposure, or both. In situations when a different product cannot be used, you can still reduce the hazard by taking steps to reduce your exposure.
Hazard = Toxicity x Exposure
 The greatest exposure hazard usually occurs while mixing and loading concentrated pesticides. Hazards associated with the actual application are frequently much lower when diluted pesticides are handled or applied. The hazards may still be substantial, however, in the case of a single high exposure (such as when an accident occurs) or when many smaller exposures occur over an extended period.
The greatest exposure hazard usually occurs while mixing and loading concentrated pesticides. Hazards associated with the actual application are frequently much lower when diluted pesticides are handled or applied. The hazards may still be substantial, however, in the case of a single high exposure (such as when an accident occurs) or when many smaller exposures occur over an extended period.
The best way to reduce or avoid the risks of pesticides is to understand the products that you are using and know how to handle and apply them safely. Read the label carefully and follow its instructions. Your attitude is most important. If you assume that you know exactly how to use a pesticide without reading the product label or do not bother to take the precautions indicated on the label, then you are more likely to experience excess exposure.
When handling pesticides, you have a legal and moral obligation to protect both your health and that of others. Besides protecting yourself, you must be aware of other people, wildlife, or pets that may be in or near the treatment area. They could be exposed to the pesticide during or after application. By following good safety practices you reduce the chance of exposure.
The pesticide registration process requires manufacturers to do risk assessment studies. They then develop product labels that provide instructions on minimizing exposure. The labels specify personal protective equipment (PPE), engineering controls, symptoms of overexposure, first aid, and post-application restricted-entry intervals (REIs).
[return]
Potential Harmful Effects of Pesticides
The two broad types of effects from pesticide exposure are: local or contact and systemic.
Local effects may occur to the area of contact with skin, eyes, or respiratory tract. They are referred to as contact symptoms or effects. Examples of local (contact) effects:
- Skin irritation or injury; itching, redness, rashes, blisters, burns, and discoloration. Many herbicides and fungicides cause dermatitis. Fumigants can cause severe blisters.
- Eye irritation or injury: swelling, stinging, and burning. Herbicides, fungicides, insecticides, and fumigants may cause eye irritation or injury through contact, sometimes resulting in irreversible damage.
- Nose, mouth, or throat irritation or injury: Swelling, stinging, and burning. Permanent respiratory damage occurs less often.
Systemic effects may occur once the substance is absorbed and distributed throughout the body. They may be acute or chronic. These effects depend on the toxicological profile of the chemical itself, the amount absorbed, and the individual's ability to detoxify and eliminate the chemical. Examples of systemic effects are:
- Damage to nerves.
- Reduced ability of blood to clot.
- Some cancers.
- Reproductive problems.
- Impaired metabolism (the body's ability to use energy).
- Hormonal effects.
- Damage to various organ systems, such as the kidneys or liver.
The U.S. Environmental Protection Agency (EPA) considers local and systemic effects when deciding whether to register a chemical. They are also used to set label restrictions, such as limiting the method, timing, or rate of application; to determine appropriate levels of PPE; or to establish restricted entry intervals (REIs) in combination with exposure factors.
Allergic effects are harmful effects that occur in some people after exposure to certain substances. An allergy to a chemical contained in a product formulation may cause skin irritation, blisters, or hives. Occasionally, more serious problems, such as asthma or even life-threatening shock can develop.
Pesticide allergy symptoms include red and/or itchy eyes, respiratory discomfort, and asthma-like effects. Unfortunately, there is no way to predict which people will develop allergies to a particular product. Having an allergic reaction does not predict whether someone would also be more sensitive to other effects of the pesticide, such as chronic or delayed effects. These types of effects depend on different chemical reactions within the body.
[return]
Exposure -- How Pesticides Get Into the Body
Pesticide exposure occurs when pesticides get onto or into the body. The four primary routes of exposure are:
Skin or Dermal Route
 Usually, the skin is the main route of entry onto or into the body. Up to 97% of all body exposure to pesticides during a spraying operation is by skin contact. Dermal absorption or contact injury may occur from airborne dust, splashes, spills, or spray mist when mixing, loading, applying, or disposing of pesticides. Skin exposure may also result from contact with pesticide residues on treated surfaces or contaminated equipment during cleaning, adjustment, or repair.
Usually, the skin is the main route of entry onto or into the body. Up to 97% of all body exposure to pesticides during a spraying operation is by skin contact. Dermal absorption or contact injury may occur from airborne dust, splashes, spills, or spray mist when mixing, loading, applying, or disposing of pesticides. Skin exposure may also result from contact with pesticide residues on treated surfaces or contaminated equipment during cleaning, adjustment, or repair.
Once a pesticide contacts the body, absorption, penetration, and distribution depend on: *chemical properties of the pesticide product, *the area of contact and rate of absorption, and *the body’s own detoxification and elimination capabilities. Some products that cause systemic injury are just as toxic when absorbed through the skin as when they are when swallowed.
Parts of the body differ in their ability to absorb pesticides. Warm, moist areas, such as the groin, armpits, head, neck, backs of the hands, and tops of the feet, tend to absorb more than the palms and forearms. However, palms and forearms must still be protected because they get the most exposure. Cuts, abrasions, and skin rashes can increase absorption. The rate of absorption (i.e., how quickly the pesticide can get into the body) differs depending on the area contacted but entry also depends on time. The longer a pesticide (or any other chemical) remains in contact, the more will be absorbed. Skin protection is important even if the area of the body most likely to contact a pesticide has a low absorption rate.
Pesticide formulations penetrate the skin at different rates. In general, wettable powders, dusts, and granular pesticides do not enter easily. However, oil-based liquid formulations, such as emulsifiable concentrates, are readily absorbed. Application techniques may also affect exposure levels for applicators. Making overhead applications, using blower application equipment for mists and dusts, are application methods that often have high dermal exposure levels. Additionally, contaminated hands or gloves can transfer pesticides to other body parts. Be sure to wash your hands and gloves after each pesticide-handling activity.
Eyes or Ocular Route
 Pesticides can be absorbed quickly and easily into the blood vessels that lie very close to the surface of the eye. In addition, corrosive products can cause severe eye damage or even blindness. Pesticides can get into your eyes as airborne dusts or particles, splashes or spills, broken hoses, spray mists, or from rubbing the eyes with contaminated hands or clothing.
Pesticides can be absorbed quickly and easily into the blood vessels that lie very close to the surface of the eye. In addition, corrosive products can cause severe eye damage or even blindness. Pesticides can get into your eyes as airborne dusts or particles, splashes or spills, broken hoses, spray mists, or from rubbing the eyes with contaminated hands or clothing.
Breathing or Inhalation Route
Protect your lungs when mixing, loading, or applying pesticides, particularly in confined areas. In sufficient amounts, inhaled pesticides can cause contact damage to sensitive tissues. They can enter the bloodstream very rapidly from the lungs, eventually damaging other body organs (systemic illness). Also, petroleum solvents in emulsifiable concentrate formulations can enter the lungs while vomiting.
Swallowing or Oral Route
 Oral exposure can occur when liquid concentrates splash into the mouth during mixing and loading of pesticides or while cleaning equipment. Never use your mouth to clear a spray line or to begin siphoning a pesticide. Eating, drinking, or smoking without first washing your hands may transfer product to your mouth. People are most likely to accidentally swallow pesticides that are improperly stored in the home or transferred into unlabeled bottles or containers normally used for food or beverages. Unfortunately, children are the most common victims of these mishaps.
Oral exposure can occur when liquid concentrates splash into the mouth during mixing and loading of pesticides or while cleaning equipment. Never use your mouth to clear a spray line or to begin siphoning a pesticide. Eating, drinking, or smoking without first washing your hands may transfer product to your mouth. People are most likely to accidentally swallow pesticides that are improperly stored in the home or transferred into unlabeled bottles or containers normally used for food or beverages. Unfortunately, children are the most common victims of these mishaps.
Clearly mark all cups and containers used to measure pesticides and store them separately from devices used to measure food and beverages. Never store pesticides in drink or food containers. Practice good personal hygiene and wear proper protective equipment. Preventing exposure is key to the safe use of pesticides.
[return]
Product Toxicity and Health Concerns
Historically, the toxicity of pesticides has been determined by subjecting test animals (usually rats, mice, rabbits, or dogs) to various dosages of the active ingredients and to each formulated product. Acute and chronic toxicity from exposure is evaluated at a range of doses: those that cause no immediate effects, those that cause some immediate effects, those that cause delayed or long-term effects, and those that cause death.
Single doses are given to assess effects from a one-time exposure. Other tests involve dosing the animals over several years to simulate exposure to small amounts throughout a lifetime. These tests can detect many different types of toxic effects ranging from subtle changes, such as weight loss or gain (which could indicate underlying problems), to specific illnesses, to death. Today, agencies that regulate pesticides are developing tests that can identify and predict the same toxic endpoints as the earlier tests required. The newer methods use mathematical models and techniques without animal testing.
Acute toxicity is the measure of harm (systemic or contact) caused by a single exposure event. Acute effects are determined after test animals have been exposed to a chemical through contact with their skin and eyes, through inhalation, or through ingestion. The harmful effects may be systemic or contact in nature (or a combination of both), depending on the product, formulation, dose, and route of exposure. Acute effects occur shortly after exposure, usually within 24 hours.
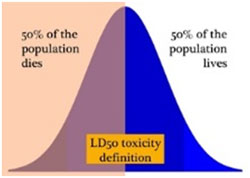 The common method used for comparing acute toxicity is the LD50, or lethal dose 50%.
The common method used for comparing acute toxicity is the LD50, or lethal dose 50%.
This is the dose of a toxicant required to kill 50% of the population of test animals under a standard set of conditions. For comparison purposes, LD50 values of pesticides are recorded in milligrams of toxicant per kilogram of body weight of the test animal (mg/kg). When the animal is exposed to material by feeding, the result is referred to as the oralLD50. When the material is tested by skin exposure, the result is called the dermal LD50.
Another commonly used measure of acute toxicity is the LC50, or lethal concentration 50%. This is the concentration of a substance in air or water required to kill 50% of the test population. It is usually expressed in parts per million or milligrams per liter (mg/l). The LC50 is a common measure of lethal effects of chemicals on fish and other aquatic organisms. The LC50 values most directly applicable to human health are those expressing lethal concentration of chemicals in the air.
The LD50 and LC50 values are useful in comparing the systemic toxicity of different active ingredients as well as different formulations of the same active ingredient. The lower the LD50 value of a pesticide, the less it takes to kill 50% of the population of test animals and the greater the toxicity of the chemical. LD50 and LC50 values have limitations because they measure only one toxic effect - death. They do not indicate what dose may lead to other, less serious acute systemic effects or to other, possibly equally serious contact or delayed systemic effects. Also, they do not translate directly to humans because our body systems are different from those of test animals. Lastly, the LD50 and LC50 are measures of a single exposure, not the potential sequence of effects resulting from multiple exposures.
Some pesticides produce acute toxic effects because of their corrosive or irritant properties. These can result in respiratory, skin, or eye irritation or damage. Some can cause severe burns or permanent blindness. Chemicals with these irritant or corrosive properties require extra care and special PPE. Fungicides, herbicides, and some insecticides may cause contact injuries. Manufacturers list nonlethal systemic and contact effects in addition to the signal word. Systemic and contact acute toxicity concerns are indicated by the signal word. They are further explained in the "Precautionary Statements" portion of the product label under the "Hazards to Humans and Domestic Animals" section.
EPA and the manufacturer take into account both systemic and contact toxicity measures in assigning the signal word and toxicity category to a product. These are assigned on the basis of the greatest concern-be it oral, dermal, or inhalation systemic effects or skin, eye, or respiratory tract contact effects.
[return]
Signal Words and Skull and Crossbones Symbol
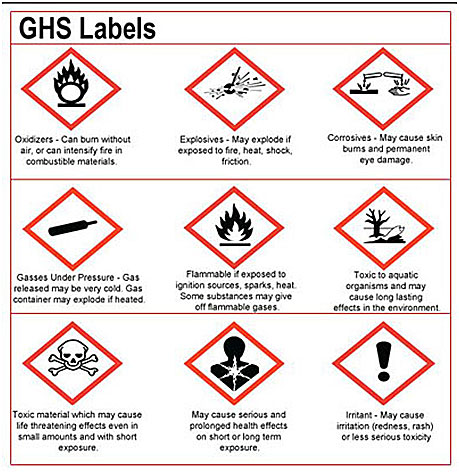
The Globally Harmonized System (GHS) for classification and labeling of chemicals is an international system for hazard communication. The goal is to improve and simplify hazard communication and alert users to the need to minimize exposure and risk. The system will identify more types of hazards than the current signal words on pesticide labels. For instance, separate pictograms and/or signal words will provide information about chronic toxicity as well as acute toxicity. This should result in safer transportation, handling, and use of chemicals.
This table summarizes the range of LD50 and LC50 values and their relationship to the different toxicity levels.
| Signal Word & Symbol | Toxicity Level & Class | LD50 Oral (mg/kg) | LD50 Dermal (mg/l) | LC50 Inhalation (mg/kg) | Toxicity Concern |
|---|---|---|---|---|---|
| DANGER-POISON/
PELIGRO Skull & Crossbones |
Highly toxic, Hazard Class I | Trace to 50 | Trace to 200 | Trace to 0.2 | a few drops to 1 teaspoon could kill |
| DANGER/ PELIGRO | Highly toxic, Hazard Class I | Based on corrosive or irritant properties of the product | |||
| WARNING/ AVISO | Moderately toxic, Hazard Class II | 50 to 500 | 200 to 2,000 | 0.2 to 2 | *1 teaspoon to 1 ounce |
| CAUTION | Slightly toxic, Hazard Class III | 500 to 5,000 | 2,000 to 20,000 | 2 to 20 | *1 ounce to 1 pint or 1 pound |
| CAUTION or no signal word | Hazard Class IV | Greater than 5,000 | Greater than 20,000 | Greater than 20 | Slight to none |
| * could cause death, illness, or skin, eye, or respiratory damage | |||||
DANGER- POISON, DANGER, WARNING, and CAUTION, the four distinct signal words currently found on pesticide labels, are based on the acute toxicity of the product. Depending on their acute toxicity, pesticide products are categorized into several hazard classes. Some very low toxicity products (Hazard Class IV) are not required to have a signal word.
Danger-Poison plus a skull and crossbones

appears on pesticides classified as highly toxic. The lethal toxicity may be based on oral, dermal, or inhalation exposure, depending on the exposure route that presents the greatest risk for that product. Consult the precautionary statements that follow the signal word and symbol on the label to learn more about the product's hazard to humans. Most fumigants, some insecticides and rodenticides, and a few herbicides are assigned the DANGER-POISON signal word.
Danger (without the word "poison" or the skull and crossbones symbol)
indicates the potential for permanent or severe damage to skin, eyes, or lungs from contact exposure. The contact effects of these pesticides are more dangerous than the acute systemic toxicity. Several carry warnings of concern about the products' ability to cause irreversible eye damage at low exposures. Consult the precautionary statements that follow the signal word on the label to learn more about the products' hazard for humans. Some herbicides, insecticides, and antimicrobials carry the DANGER signal word.
Warning
signal word alone does not indicate whether the concern is systemic, contact, or both. Consult the precautionary statements that follow the signal word on the label to learn about the product's specific contact or systemic hazard for humans.
Caution
Contact effects are generally irritation of eyes, skin, or respiratory tract. Consult the precautionary statements that follow the signal word on the label to learn about the product's contact or systemic hazard to humans.
[return]
Chronic Toxicity
The chronic toxicity of a pesticide is determined by subjecting test animals to long-term (usually 2 years) exposure to an active ingredient. The harmful effects that occur from small, repeated doses over time are termed chronic effects.
Chronic effects from pesticide exposure include genetic changes, noncancerous or cancerous tumors, reproductive effects, infertility, fetal toxicity, miscarriages, birth defects, blood disorders, nerve disorders, and hormonal or endocrine-mediated diseases. Each pesticide has its own characteristic pattern of diseases and adverse effects that it might cause. However, no single pesticide is likely to be able to cause the entire range of harmful effects. Minimizing the likelihood of chronic effects is one of the important reasons to follow all label directions and be cautious in handling and applying pesticides.
If a product causes chronic effects in laboratory animals, the manufacturer is required to include chronic toxicity warning statements on the product label. This information is also listed on the Safety Data Sheet. The chronic toxicity of a pesticide is more difficult to determine through laboratory analysis than the acute toxicity and cannot be expressed by a single measure.
[return]
Delayed Effects
Delayed effects are illnesses or injuries that do not appear immediately (within 24 hours) after exposure to a pesticide. They may be delayed for weeks, months, or even years. Whether you experience delayed effects depends on the pesticide, the extent and route of exposure(s), and how often you were exposed. The "Precautionary Statements" section of the label states any delayed effects that the pesticide might cause. It also tells you how to avoid exposures. Delayed effects may be caused by either an acute or a chronic exposure to a pesticide.
[return]
Factors Affecting Response
 Humans have built-in mechanisms to reduce the risks of toxic substances and to eliminate them from the body. The liver is the primary organ that changes toxic substances to nontoxic or less-toxic forms. Its chemical breakdown processes help to make most of these substances more water-soluble so they can be eliminated.
Humans have built-in mechanisms to reduce the risks of toxic substances and to eliminate them from the body. The liver is the primary organ that changes toxic substances to nontoxic or less-toxic forms. Its chemical breakdown processes help to make most of these substances more water-soluble so they can be eliminated.
The kidneys filter water-soluble unwanted chemicals out of the blood and into the urine. Those that cannot be made water-soluble are eventually are stored in fatty deposits throughout the body and in breast milk. Many of the pesticides in use today are more water-soluble than those used before 1970. Most are eliminated relatively quickly (hours to days instead of months to years) in urine.
Some pesticides can cause changes, called mutations, to our DNA. DNA is the carrier of genetic information in our bodies. Some DNA mutations do not cause any effects. Others cause serious malfunctions and may lead to various types of illnesses or other problems, such as birth defects. Although our bodies constantly monitor and repair DNA mutations, over time our ability to repair the DNA decreases. Our bodies continually manufacture the enzymes we need to help detoxify pesticides and other toxic substances. However, continual or very frequent exposures may overwhelm the body's capacity for chemical breakdown and elimination. Keeping your exposure low and having periods of non-exposure between applications of the same class of pesticide can reduce the chance that your body will be overwhelmed.
[return]
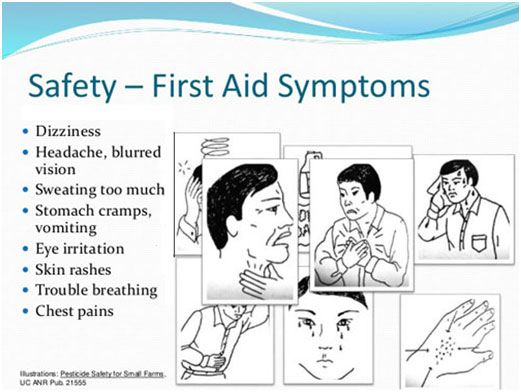
Symptom Recognition
Symptoms can be correlated with certain groups of pesticides. For example, some fungicides irritate the skin, eyes, and mucous membranes of the respiratory system. Symptoms associated with synthetic pyrethroid insecticides include nausea, dizziness, weakness, nervousness, and eye and skin irritation. Chlorophenoxy herbicides, such as 2,4-D and some related products (dicamba, MCPA, and MCPP) irritate the skin and mucous membranes. They may also cause vomiting, headaches, diarrhea, and confusion.
[return]
First Aid for Pesticide Poisoning
Get medical advice immediately for unusual or unexplained symptoms that develop within 24 hours of a pesticide exposure. Be alert for the early symptoms of pesticide poisoning and contact (local) effects in yourself and others. Do not wait to call a physician until you or someone else gets dangerously ill. It is better to be too cautious than to act too late.
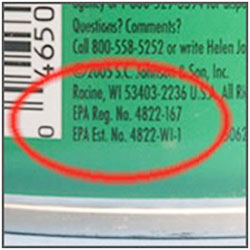 Take the pesticide label or EPA registration number with you to help medical personnel to treat you appropriately and quickly. The label is important because the medical professional needs to know the pesticide ingredients to determine the proper course of treatment. It is a good idea to print off extra copies of the label from the Internet. Place one copy in your service vehicle and one in your office in case of a medical emergency.
Take the pesticide label or EPA registration number with you to help medical personnel to treat you appropriately and quickly. The label is important because the medical professional needs to know the pesticide ingredients to determine the proper course of treatment. It is a good idea to print off extra copies of the label from the Internet. Place one copy in your service vehicle and one in your office in case of a medical emergency.
Keep in mind that symptoms commonly associated with certain pesticides are not always the result of exposure. Common illnesses (e.g., the flu, heat exhaustion or heatstroke, pneumonia, asthma, respiratory or intestinal infections, and even a hangover) can cause symptoms similar to those of many frequently used pesticides. Contact with certain plants, such as poison oak or poison ivy, may also produce skin effects like those resulting from pesticide exposure. However, it is best to take every precaution. When symptoms appear after contact with pesticides, always seek medical attention immediately.
General First Aid
First aid is the initial effort to assist a victim while medical help is on the way. If you are alone with the victim, make sure he or she is breathing and exposure to the pesticide has stopped. Then call for help. Protect yourself from pesticide exposure before and while giving assistance. Make sure you wear the appropriate PPE, including a respirator if indicated, before assisting someone in an enclosed area. Administer artificial respiration if the victim is not breathing and is not vomiting.
Immediate action can be a life-or-death matter in a pesticide poisoning. The product label is the primary source of information. Follow the label's specific first aid instructions carefully. Beyond the label, call the American Association of Poison Control Centers (AAPCC) (800-222-1222) or a physician for additional advice. It is very important to get the victim to a hospital, or contact 911 for emergency response, without delay. Post all emergency numbers near telephones and in service vehicles used by pesticide handlers.
Key points to remember when administering first aid during a pesticide emergency:
Oral or dermal exposure:
- Remove all contaminated clothing immediately.
- Rinse the exposed area with water to dilute the pesticide and to prevent skin absorption. Use the cleanest water available.
- Wash the affected area, including the hair, with water and soap. Then, rinse well. Showering is better than bathing to avoid prolonged contact with pesticide residues. Avoid harsh scrubbing, which could damage the skin and enhance pesticide absorption. Gently dry the affected area and wrap it in loose cloth or a blanket, if necessary.
- If the skin has chemical burns, cover the area loosely with a clean, soft cloth. Do not use ointments, greases, powders, and other medications unless instructed to do so by a medical authority.
- Never try to give an unconscious person anything by mouth.
- Do not induce vomiting unless the label tells you to.
- If inhalation exposure has occurred, get the victim to fresh air immediately.
- Become familiar with the proper techniques of artificial respiration. It may be necessary if a person's breathing has stopped or becomes impaired.
- If first responders are likely to be directly exposed to a pesticide, be sure they wear appropriate PPE.
Pesticide in the Eyes
- Because eyes readily absorb material, fast action is required.
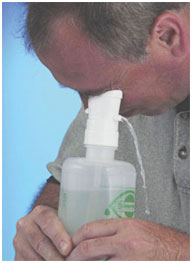
- Hold the eyelid open and immediately begin gently washing the eye with drips of clean water. Do not use chemicals or drugs in the wash water unless instructed to do so by a medical professional or a poison control center.
- Drip the water across-not directly into-the eye, or use an eyewash dispenser.
- Continuously rinse the eye for 15 minutes. If only one eye is affected, be careful not to contaminate the other eye.
- Flush under the eyelid with water to remove debris.
- Cover the eye with a clean piece of cloth and seek medical attention immediately.
Inhaled Pesticide
- Immediately carry the victim to fresh air (do not allow him or her to walk).
- Do not attempt to rescue someone who is in an enclosed, contaminated area unless you are wearing appropriate PPE.
- Warn other people in the area of the danger.
- Have the victim lie down and loosen his or her clothing.
- Keep the victim warm and quiet. Do not allow him or her to become chilled or overheated.
- If the victim is convulsing, protect his or her head, turn the head to the side, and watch that breathing continues. Do not attempt to insert anything into the person's mouth during a seizure.
- Keep the person's chin up to ensure that air passages are open for breathing.
- Give artificial respiration if breathing stops or is irregular,.
Pesticide in the Mouth or Swallowed
- If pesticide is in someone's mouth but has not been swallowed, rinse the mouth with plenty of water. Then, give the victim large amounts (up to 1 quart) of milk or water to drink.
- If the pesticide is swallowed, one of the most critical first aid decisions is whether to induce vomiting. Induce vomiting only if the label instructs you to do so. Several pesticides cause more harm when vomited than if they remain in the stomach. To provide first aid for a swallowed pesticide, you must know the appropriate treatment. The decision to induce vomiting must be made quickly and accurately-the victim's life may depend on it.
Never induce vomiting if the victim:
- Is unconscious or having convulsions.
- Has swallowed a corrosive poison, such as a strong alkali or acid. The material burns the throat and mouth as severely coming up as it did going down. Also, it can be aspirated into the lungs and cause more damage.
- Has swallowed an emulsifiable concentrate or oil solution product, which is dissolved in petroleum solvents. Emulsifiable concentrates and oil solutions may be fatal if aspirated into the lungs during vomiting.
[return]
Heat Stress
Heat stress occurs when the body cannot cope with a certain level of heat. Heat stress may affect both pesticide handlers and other workers. A person suffering from heat stress exhibits symptoms that closely resemble poisoning symptoms of some pesticides.
PPE worn during handling or early-entry activities may increase the risk of heat stress. its protective qualities may restrict the evaporation of sweat, interfering with the body's natural cooling system. If you are under a physician's care, consult him or her before working in hot or humid conditions. Vests and headbands with special pockets for ice packs or other heat stress prevention devices may be worn with or beneath PPE. These will help maintain a cool body temperature.
Symptoms of Heat Stress
Mild forms of heat stress make people feel ill and impair their ability to do a good job. You may feel weak and get tired sooner than usual. You may also be less alert and less able to use good judgment.
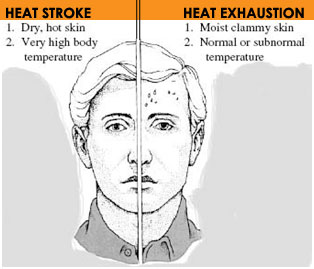
Severe heat stress, also known as heatstroke, is life-threatening. The normal human body temperature ranges from about 97°F to 99°F, with an average of 98.6°F. With heatstroke, body temperature may exceed 105°F. Staggering, loss of consciousness or convulsions may result. Lack of sweating is a common symptom of heatstroke. Brain damage or even death may occur if the heatstroke victim is not cooled very quickly. More than 10% of severe heat stress victims die-including young, healthy adults. Sometimes victims remain highly sensitive to heat for months and cannot return to the same type of work.
Heat stress symptoms include:
- Fatigue, exhaustion, or muscle weakness
- Dizziness and fainting
- Clammy or hot, dry skin
- Altered behavior: confusion, slurred speech, quarrelsome or irrational conduct
- Headache, nausea, and chills
- Severe thirst and dry mouth
- Heavy sweating: eventually, this can progress to a complete lack of sweating as the body loses the ability to control its temperature
Act immediately to cool down if you suspect that you may be suffering from even mild heat stress. Drink plenty of water and take breaks in the shade throughout the workday. In hot conditions, watch for symptoms of heat stress in other workers as well.
[return]
Summary
Pesticide risk can be summarized by the equation hazard (risk) = toxicity x exposure.
Hazard = Toxicity x Exposure
"Toxicity" is the capacity of the pesticide to cause either short-term (acute) or long-term (chronic) injury or illness; "exposure" is the means by which the pesticide gets into or onto the body. These two factors determine the likelihood that harm (i.e., hazard) will come to a person who handles pesticides.
Harmful effects of pesticides may occur at the area of local contact or after uptake into the body (i.e., systemic effects). Pesticides can enter the body by any of four routes: through the skin (dermal), eyes (ocular), lungs (respiratory), or mouth (oral). Some adverse effects may occur within 24 hours after a single (usually large) exposure (acute effects). Others may occur many years after exposure (delayed effects), typically from small exposures over a long period (chronic effects). Pesticide handlers can minimize exposure-and reduce risk-by following label directions, using the proper application and handling procedures, and wearing appropriate personal protective equipment.
The toxicity of a pesticide product is measured in test animals by the LD50 and LC50 values. These values determine the signal word that occurs on the pesticide label. Signal words- DANGER-POISON, DANGER, WARNING, and CAUTION-help the user recognize how acutely toxic the pesticide is and what precautions to take. Remember, however, that the signal word only provides information about the acute toxicity of the product. Chronic and delayed effects are often the result of different mechanisms and are not related to the substance's level of acute toxicity.
People who use pesticides routinely should have regular medical checkups to determine if they are experiencing any ill effects from pesticide use. Regular monitoring of blood cholinesterase levels can determine if certain insecticides are affecting an individual before symptoms appear.
Early recognition of pesticide poisoning symptoms is the key to preventing further injury. The label often provides important information on first aid procedures for the particular pesticide product. Make sure a copy of the label is readily available whenever you are using pesticides. Take the label to a medical professional if a poisoning incident occurs.
[return]
1) The minimum personal protective equipment (PPE) needed to reduce exposure to a pesticide is listed in the ____ of the product label.
- General directions for use
- Precautionary statements
- Specific directions for use
- Storage and disposal
2) The hazard or risk to human health from a pesticide depends on its toxicity and the __________.
3) These formulations of a pesticide (WP, EC, G, etc.) have the same risk of exposure to the applicator.
4) The greatest pesticide exposure hazard to an applicator occurs during ______.
- mixing and loading of concentrates
- sprayer calibration
- changing sprayer nozzles
- rinsing the sprayer after an application
5) Which one of the following is an example of a "local effect" of pesticide exposure?
6) Which of the following is an example of a "systemic effect" of pesticide exposure?
7) Hives, blisters, or skin irritation are examples of which one of the following pesticide exposure effects?
8) Over 90% of all body exposures while spraying are due to _____ contact with the pesticide.
9) Which one of the following sites on a human body absorbs the greatest percentage of a pesticide dose?
10) Skin cuts, scrapes, or rashes _______ the absorption of a pesticide into the body.
11) ______ formulations of a pesticide will be absorbed most quickly into the skin.
12) Corrosive pesticide formulations pose the greatest risk of damage to the _______.
13) Which formulation poses the greatest risks to a person who has vomited after accidentally ingesting a pesticide?
14) Which one of the following is used to express the dose of a chemical that will kill 50% of the test organisms?
15) Which one of the following LD50’s is most toxic?
16) An LC50 value for a pesticide measures _______ of the test subject.
17) Contact and systemic effects of pesticides are explained in the _______ section of a pesticide label.
- General directions for use
- Precautionary statements
- Specific directions for use
- Storage and disposal
18) The words _________ appear on the labels of pesticides that are highly toxic.
19) A pesticide with the signal word _______ indicates the potential for permanent or severe damage to skin, eyes, or lungs from contact exposure.
20) Chronic toxicity effects of pesticide exposure occur after ________ of exposure.
21) Which of the following is a potential chronic effect of pesticide exposure?
22) The _____ is the primary organ that changes toxic substances to non-toxic substances so that they can be eliminated from the body.
23) The _____ filters water-soluble chemicals from the blood for removal in the urine.
24) Get medical advice within ______ of experiencing unusual or unexplained symptoms following a pesticide exposure.
25) Which of the following is most useful to medical personnel who are treating a person for pesticide exposure?
- product’s EPA registration number
- product sales brochure
- dealer's telephone number
- your supervisor’s telephone number
26) Which of the following is NOT a potential symptom of pesticide poisoning?
27) What should be done with clothing that has been heavily contaminated by a pesticide concentrate?
28) If a pesticide splashes into the eyes, rinse them for _____ .
29) Usually, the first thing to do for a person with concentrated pesticide on their skin is to _______.
- induce vomiting
- wash the area gently with soap and water
- scrub the area with a stiff brush to remove contaminated skin
30) If a person has a chemical burn from pesticide exposure, you should cover the area with a thick layer of ointment or grease.
31) The symptoms of heat stress can resemble those of pesticide poisoning.
32) Lack of sweating is a common symptom of heatstroke.
33) The signal word on a pesticide label give you information about the product’s acute and chronic toxicity.
website content by L. Townsend website designed by P.M. Dillon copyright © 2015 University of Kentucky Department of Entomology
University of Kentucky College of Agriculture |
S-225 Agricultural Science Center North, Lexington, KY 40546-0091 | 859.257.7450
An Equal Opportunity University |
Last modified
11/30/2018
