TOPICS
- Home
- Challenges
- EIA Virus
- Transmission NEW!!
- Persistent Infection
- Pathogenesis
- Immune Response
- Diagnosis & Control
- Field Studies
- Publications NEW!!
- Links
- Contact and Credits
HOT TOPICS IN EIA RESEARCH
Disease Pathogenesis
The following will appear in the Equine Veterinary Journal article, authored by Cook RF, Cook SJ, Issel CJ, as a part of an infectious diseases monograph issue due out in 2009:
"Pathogenesis of Disease"
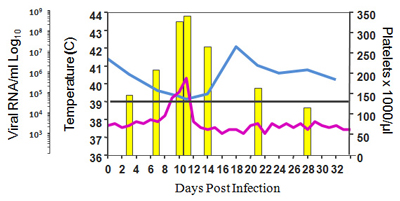
In animals infected with EIAV, there is a very close relationship between overt signs of disease and amounts of virus present (see Figure below).
Tissue associated viral burdens are at their highest levels during febrile episodes and decline several orders of magnitude concomitant with the resolution of clinical signs. It has been demonstrated that amounts of tissue-associated EIAV must reach a critical or threshold value in order to trigger disease (Cook et al. 2003). The observed variation in clinical signs may therefore be interpreted in the context of threshold viral burdens. Following acute infection, disease in normal, fully immunocompetent horses will only be produced if the inoculum strain of EIAV reaches or exceeds the threshold viral burden level before primary immune responses effectively limit viral replication. Therefore, to induce disease the infecting virus must possess sufficient replicative potential within its host. Although the spectrum of virulence among naturally occurring EIAV strains has not been rigorously determined it is known that any mutation in the viral genome that reduces viral replication rates in vivo will attenuate pathogenicity (Cook et al. 2003; Cook et al. 1998; Threadgill et al. 1993; Lichtenstein et al. 1995). In addition to viral replicative ability, differences between individual animals and between species of equid also play a significant role in the appearance of clinical signs following infection with EIAV. For example, in an experiment involving infection of horses/ponies with identical amounts of a pathogenic strain of EIAV derived from an infectious molecular clone it was observed some animals could control acute viral replication more efficiently and as a result had no obvious disease signs (Cook et al. 2003). Furthermore, a comparison between different species of equid infected with horse virulent EIAV strains showed that donkeys remained clinically unaffected and that their peak viral titers were at least a 1000-fold lower than in horses or ponies (Cook et al. 2001). A supplemental conclusion from research in different species is that once EIAV has been adapted to one equid host it may not replicate optimally in another species of equid.
Many of the clinical signs associated with acute EIA are caused by pro-inflammatory mediators released in response to tissue associated viral burdens reaching the threshold level and are not dependent on the development of viral-specific adaptive immune responses. This is demonstrated by the fact acute EIA signs occur in foals that lack mature T or B cells because of inherited Severe Combined Immunodeficiency (SCID) disease (Crawford et al. 1996; Tornquist et al. 1997) . The pathology of lentiviral-mediated disease is augmented by the fact that infection of macrophages by this group of viruses disrupts the regulation of host-cell gene expression to produce increases in the production of pro-inflammatory molecules such as tumor necrosis factor alpha (TNFα), interleukin 1 (IL-1α and IL-1β) and interleukin 6 (IL-6) (Yoo et al. 1996; Esser et al. 1996; Lechner et al. 1997; Lim et al. 2005; Swardson et al. 1997). This has been demonstrated in equine monocyte-derived macrophage cultures where infection with pathogenic strains of EIAV produces significant increases in the production of these cytokines (Lim et al. 2005) and during acute disease where significantly elevated blood levels of TNFα, IL-6 and transforming growth factorβ (TGFβ) have been observed (Tornquist et al. 1997; Sellon et al. 1999; Costa et al. 1997). IL-1, IL-6 and TNFα can induce febrile responses by activating the arachidonic pathway to increase production of prostaglandin E2 (PGE2). In addition to inducing febrile reactions, the cytokines released in response to EIAV infection may also cause thrombocytopenia. For example, TNFα and TGFβ have both been shown to suppress equine megakaryocyte colony growth (Tornquist and Crawford 1997) and in the mouse model injection with TNFα alone induces a profound thrombocytopenia by stimulating cells expressing the widely distributed 55 kDa Tumor Necrosis Factor Receptor 1 (TNFR1) to release platelet agonists such as thrombin, plasmin and serotonin (Tacchini-Cottier et al. 1998). Excessive TNFα production may also contribute to anemia in EIAV infected animals because it has the ability to suppress erythropoiesis (Felli et al. 2005; Zamai et al. 2000; Dufour et al. 2003; Moldawer et al. 1989). However, it is not the only mechanism because extensive phagocytosis of complement C3 coated erythrocytes also occurs in these animals, resulting in the presence of hemosiderin granules in the macrophages found in organs such as the liver, spleen and lymph nodes (Sentsui and Kono 1987; Perryman et al. 1971).
While clinical signs of acute EIA can be attributable to the storm of pro-inflammatory cytokines released in response to the burden of tissue-associated EIAV attaining the critical threshold level, adaptive immune responses, when present, also play a role in the pathogenesis of EIA. For example, platelets from EIAV infected horses have significant levels of bound IgG or IgM and so become destined for immune mediated destruction contributing to splenomegaly and hepatomegaly (Banks et al. 1972; Clabough et al. 1991). Furthermore, the glomeruli in the kidneys of chronically infected animals often show thickening of the glomerular tufts with both mesangial and epithelial cell proliferation. These diseased glomeruli have both immunoglobulin and complement C3 deposited at the basement membranes and mesangial areas (Henson and McGuire 1971).
References:
- Cook RF, Leroux C, Cook SJ, Berger SL, Lichtenstein DL, Ghabrial NN, Montelaro RC, Issel CJ (1998) Development and characterization of an in vivo pathogenic molecular clone of equine infectious anemia virus. J Virol, 72: 1383-93.
- Cook SJ, Cook RF, Montelaro RC, Issel CJ (2001) Differential responses of Equus caballus and Equus asinus to infection with two pathogenic strains of equine infectious anemia virus. Vet Microbiol, 79: 93-109.
- Cook RF, Cook SJ, Berger SL, Leroux C, Ghabrial NN, Gantz M, Bolin PS, Mousel MR, Montelaro RC, Issel CJ (2003) Enhancement of equine infectious anemia virus virulence by identification and removal of suboptimal nucleotides. Virology, 313: 588-603.
- Crawford TB, Wardrop KJ, Tornquist SJ, Reilich E, Meyers KM, McGuire TC (1996) A primary production deficit in the thrombocytopenia of equine infectious anemia. J Virol, 70: 7842-50.
- Costa LR, Santos IK, Issel CJ, Montelaro RC (1997) Tumor necrosis factor-alpha production and disease severity after immunization with enriched major core protein (p26) and/or infection with equine infectious anemia virus. Vet Immunol Immunopathol, 57: 33-47.
- Dufour C, Corcione A, Svahn J, Haupt R, Poggi V, Beka'ssy AN, Scime R, Pistorio A, Pistoia V (2003) TNF-alpha and IFN-gamma are overexpressed in the bone marrow of Fanconi anemia patients and TNF-alpha suppresses erythropoiesis in vitro. Blood, 102: 2053-9.
- Esser R, Glienke W, von Briesen H, Rubsamen-Waigmann H, Andreesen R (1996) Differential regulation of proinflammatory and hematopoietic cytokines in human macrophages after infection with human immunodeficiency virus. Blood, 88: 3474-81.
- Felli N, Pedini F, Zeuner A, Petrucci E, Testa U, Conticello C, Biffoni M, Di Cataldo A, Winkles JA, Peschle C, De Maria R (2005) Multiple members of the TNF superfamily contribute to IFN-gamma-mediated inhibition of erythropoiesis. J Immunol, 175: 1464-72.
- Issel CJ, Cook SJ, Howell D, Nitschke Sinclear J, Gardner D, Mathis JG, Marshall MR, Rogers LE. (1998) Equine infectious anemia in wild free-roaming horses in Utah. US An. Health Assn. Proc. 102, 376-384.
- Lechner F, Machado J, Bertoni G, Seow HF, Dobbelaere DA, Peterhans E (1997) Caprine arthritis encephalitis virus dysregulates the expression of cytokines in macrophages. J Virol, 71: 7488-97.
- Lichtenstein DL, Rushlow KE, Cook RF, Raabe ML, Swardson CJ, Kociba GJ, Issel CJ, Montelaro RC (1995) Replication in vitro and in vivo of an equine infectious anemia virus mutant deficient in dUTPase activity. J Virol, 69: 2881-8.
- Lim WS, Payne SL, Edwards JF, Kim I, Ball JM (2005) Differential effects of virulent and avirulent equine infectious anemia virus on macrophage cytokine expression. Virology, 332: 295-306.
- Moldawer LL, Marano MA, Wei H, Fong Y, Silen ML, Kuo G, Manogue KR, Vlassara H, Cohen H, Cerami A, et al (1989) Cachectin/tumor necrosis factor-alpha alters red blood cell kinetics and induces anemia in vivo. FASEB J, 3: 1637-43.
- Perryman LE, McGuire TC, Banks KL, Henson JB (1971) Decreased C3 levels in a chronic virus infection: equine infectious anemia. J Immunol, 106: 1074-8.
- Sellon DC, Russell KE, Monroe VL, Walker KM (1999) Increased interleukin-6 activity in the serum of ponies acutely infected with equine infectious anaemia virus. Res Vet Sci, 66: 77-80.
- Sentsui H, Kono Y (1987) Phagocytosis of horse erythrocytes treated with equine infectious anemia virus by cultivated horse leukocytes. Arch Virol, 95: 67-77.
- Swardson CJ, Lichtenstein DL, Wang S, Montelaro RC, Kociba GJ (1997) Infection of bone marrow macrophages by equine infectious anemia virus. Am J Vet Res, 58: 1402-7.
- Tacchini-Cottier F, Vesin C, Redard M, Buurman W, Piguet PF (1998) Role of TNFR1 and TNFR2 in TNF-induced platelet consumption in mice. J Immunol, 160: 6182-6.
- Threadgill DS, Steagall WK, Flaherty MT, Fuller FJ, Perry ST, Rushlow KE, Le Grice SF, Payne SL (1993) Characterization of equine infectious anemia virus dUTPase: growth properties of a dUTPase-deficient mutant. J Virol, 67: 2592-600.
- Tornquist SJ, Crawford TB (1997) Suppression of megakaryocyte colony growth by plasma from foals infected with equine infectious anemia virus. Blood, 90: 2357-63.
- Tornquist SJ, Oaks JL, Crawford TB (1997) Elevation of cytokines associated with the thrombocytopenia of equine infectious anaemia. J Gen Virol, 78 ( Pt 10): 2541-8.
- Yoo J, Chen H, Kraus T, Hirsch D, Polyak S, George I, Sperber K (1996) Altered cytokine production and accessory cell function after HIV-1 infection. J Immunol, 157: 1313-20.
- Zamai L, Secchiero P, Pierpaoli S, Bassini A, Papa S, Alnemri ES, Guidotti L, Vitale M, Zauli G (2000) TNF-related apoptosis-inducing ligand (TRAIL) as a negative regulator of normal human erythropoiesis. Blood, 95: 3716-24.
Updated on: February 17, 2010